Should I have a tonsillectomy?
- Posted on: Dec 24 2022
Tonsillectomy is one of the oldest surgeries documented. Before the advent of modern surgery and anesthesia, it used to be done by ENT doctors performing the surgeries during a home visit. My late uncle, who used to be a big burly guy in his youth, told me stories of him having a summer job as the “anesthesiologist”. He used to follow the ENT doctor around and hold the kids steady as the ENT doctor performed the procedure going from home to home. Nowadays the procedure is performed under general anesthesia in the operating room.
The debate has always been who should and should not get a tonsillectomy. A few decades ago, most children used to routinely get a tonsillectomy even if they were not sick. The pendulum then swung to the other side, and there was a trend to not perform tonsillectomy for as long as possible. Now the pendulum is swinging back to the midline, and tonsillectomies are done for defined indications. Many adults who perhaps should have had a tonsillectomy as children are now coming back on their own still with tonsil concerns, and need to get the procedure done as an adult.
The American Association of Otolaryngology Head and Neck Surgery (AAOHNS) has published clinical practice guidelines for consideration for tonsillectomy in children. Although we don’t have similar guidelines for the adult population, many clinicians extrapolate the guidelines for all age groups.
One obvious indication for tonsillectomy is recurrent infections. Typically these are infections in which the patient has seen by their doctor, documentation of infection was made, proper medical therapy was administered, and there was loss of quality of life due to missing days at school or work. Many patients who have had a few infections believe they meet the criteria for tonsillectomy, mostly out of frustration, but actually do not qualify for the procedure. The guidelines recommend tonsillectomy if the patient had 7 or more infections in one year, 5 or more infections per year for the past 2 years, or 3 or more infections per year for the past few years. These numbers are guidelines only; they are not mandatory. In the appropriate clinical setting, the patient and their doctor may decide to proceed with surgery even if these numbers are not satisfied, or they may decide to postpone surgery even if the numbers are met.
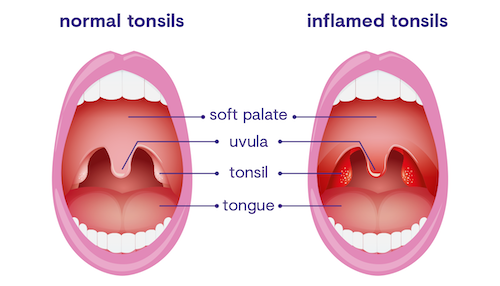
Besides conventional tonsil infections, peritonsillar abscess is another consideration for tonsillectomy. Anatomically, the tonsils are attached to the throat muscles with a very thin membrane separating them. Rarely, infections may find their way into this area of separation where there is not a good blood supply, and then the bacteria flourish. This causes the displacement of the tonsil towards the midline, partially occluding the breathing passages. The initial treatment usually involves draining the abscess, as well as a course of antibiotic. Most doctors agree that any one infection is mostly the result of bad luck. However, two or more such infections usually indicate a trend. It is recommended to consider tonsillectomy after the second bout of peritonsillar abscess infection.
Another indication for a tonsillectomy has to do with sleep disorders. These include snoring, sleep apnea, or restless sleep. Although snoring is rather easy to diagnose, we usually recommend an overnight sleep test to document the extent of sleep apnea. In patients with very large tonsils, tonsillectomy can incrementally improve the snoring and apnea, but may not necessarily eradicate the problem altogether. Occasionally additional surgeries may also need to be performed, either at the same time or at a later time. Additional measures could also be necessary in the form of device therapy or weight management.
Tonsil stones are another reason to contemplate tonsillectomy. The criteria here are much less defined. Many patients suffer from large tonsils which trap concretions within small shallow pockets. These concretions may cause bad breath, sensation of fullness in the back of the throat, problems with swallowing, and rarely causes tonsil infections. Most doctors recommend maximal medical therapy with various techniques to alleviate the symptoms. Partial or full tonsillectomy is reserved as a last resort.
A final consideration for a tonsillectomy has to do with tumors and cancers. HPV infections have become much more widespread, and the tonsils are one of the more common locations within the oral cavity for the virus to seed itself. After the passage of much time, some people experience tumor growth. Many of these lesions are clinically obvious in an office exam. If possible, a simple biopsy of the growth can be done under local anesthesia in an office setting. However, if the lesion is not accessible or if the patient has a significant gag reflex, removal of that tonsil under anesthesia might be the correct choice. If indeed a cancer is diagnosed, based on the extent of the growth and staging of the cancer, additional treatments might also be necessary besides a simple tonsillectomy.
Patients who have had issues with their tonsils and believe a tonsillectomy might be beneficial for them should consult their ear, nose and throat doctor to discuss the clinical criteria together. The majority of patients can have their tonsillectomy on an ambulatory basis and go home the same day. The recovery from a tonsillectomy is rather painful and challenging, and most patients are encouraged to allow a good amount of time for recovery at home. Patients are encouraged to discuss all the risks, benefits, and alternatives with their ENT surgeon in order to make an informed decision.
Tagged with: abscess, ear nose throat, ENT, Isaac Namdar, Isaac Namdar MD, New York, new york city, ny, NYC, Otolaryngology, Otorhinolaryngology, peritonsillar abscess, tonsil concretions, tonsil stones, Tonsillectomy, tonsillitis
Posted in: Throat